Mental Health Manifestations in a Case of Dandy-Walker Variant
Mohamed El Tahir, Ibrahim Abdelhafez, and Salma Salman
Mohamed El Tahir1*, Ibrahim Abdelhafez1 and Salma Salman2
1Department of Psychiatry, Hamad Medical Corporation, Doha, Qatar
2College of Medicine, QU Health, Qatar University, Doha, Qatar
- *Corresponding Author:
- Mohamed El Tahir
Department of Psychiatry
Senior Consultant Learning Disability Psychiatrist
Hamad Medical Corporation
Doha, Qatar
E-mail: MElTahir2@hamad.qa
Received Date: October 02, 2021; Accepted Date: October 15, 2021; Published Date: October 22, 2021
Citation: Tahir MEI, Abdelhafez I, Salman S (2021) Mental Health Manifestations in a Case of Dandy-Walker Variant. J Neuropsychiatry Vol.5 No.1: 12.
Abstract
Dandy-Walker variant disorder is a defined as cerebellar dysgenesis, enlarged posterior fossa with variation of cerebellar vermis hypoplasia and less commonly agenesis/thinning of the corpus callosum. Commonly reported symptoms in the literature are intellectual disabilities, epilepsy, and developmental delay. The pathogenesis of psychological manifestations in the illness is believed to be attributed to abnormal corticocerebellar tracts, resulting in what is recognized as cerebellar cognitive affective syndrome. Reports about the clinical manifestation and management challenges associated with Dandy-Walker variant coexisting with impulsive/destructive behavior are very few. We report a case of young adult man with Dandy-Walker variant who presented with challenging behaviors outbursts including verbal abusive, physically assaultive, environmental destruction and sexually disinhibited behavior and destructive behavior causing high risk of injury and financial consequences. His presentation suggests and organic psychosis diagnosis in the context of uncontrolled epilepsy. This report highlights the challenges in diagnostic formulation and management of this case; especially the collaboration of different services and the need of monitoring the pharmacotherapy, behavioral support plans and risk management to safeguard the patient and his family. The report also explores the possible factors contributing to the progression of his behavioral and mental health. In comparison with previously published cases.
Keywords
Intellectual disability; Challenging behavior; Epilepsy; Dandy-Walker variant
Introduction
The terms Dandy-Walker complex or Dandy-Walker Syndrome (DWS) are used to denote the commonest cerebellar congenital anomalies of the posterior fossa; malformation (DWM) (agenesis of cerebellar vermis), variant (DWV) (hypoplastic cerebellar vermis), mega cisterna magna and arachnoid cyst [1-3]. DWS impacts 1/25,000 to 1/35,000 births, with higher incidence in females [4]. The variant form lacks hydrocephalus, with decreased neurological manifestations, and better prognosis [5]. DWS has been reported to be associated with schizophrenia, bipolar disorder, psychosis, obsessive/compulsive behaviors, hyperactivity, and impulsive/destructive behaviors [6-20]. Psychiatric comorbidities such as Attention Deficit Hyperactivity Disorder have been reported with associated Intellectual Disability and challenging behaviors [12].
We report a case of an adult male with Dandy-Walker presenting with organic psychosis and complex challenging behaviors including episodes of temper tantrums; anger outbursts, verbally abusive, physically assaultive, severe destructive and sexually disinhibited behaviors associated with social avoidance. We discuss aspects of risk management and implications of wide system approach.
Case Study
An 18 years old adult male of Arabian descent living with his family and recently left school due to lack of progress and behavioral problems. He was referred to the Mental Health Service, Learning Disability clinic with history of progressive deterioration in his behaviors over a period of one and half years. His behaviors described as episodic but of high intensity starts with him making demands and escalates to becoming aggressive towards his family and attacking the environment breaking TV screens and any valuable items, he get in his hand. He has been observed by his family as becoming increasingly isolated in his room, refusing to come out during the day and only comes out at night after all goes to bed. He gets in the kitchen but often engage in breaking items and opening all food cans to throw them on the floor. He sometimes goes to his younger brother’s room and demands their phone claiming it as his phone. Attempts at managing his behavior often require his father to try containing him by force as he can put himself and others at risk during these episodes. His father continued to sleep during the day and wakes up at night to ensure safety in the house from his behaviors. When out, he attacked the cars with stones and has broken number of family and neighbor’s cars. His mood has been volatile, irritable, and easily provoked and often suspicious of all the family members leading to significant problem with relationship.
He has been seen before by child and adolescent psychiatrist, his behavioral problems were noted as social avoidance with nervousness, abnormal movements, and learning disability. He was diagnosed with anxiety and prescribed Escitalopram optimum dose with limited response and repeated episodes of challenging behaviors. His intellectual abilities were tested and his total IQ score reported as 57-60 using Wechsler Intelligence Scale for children-III (WISC-III).
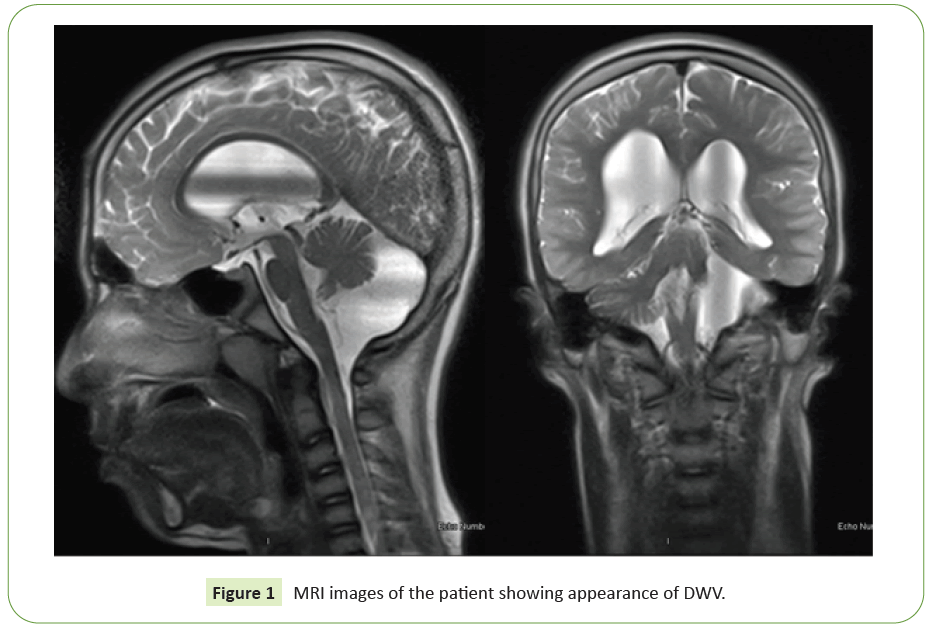
He was also a known case of Epilepsy diagnosed by neurologist at age 12 years and was kept on antiepileptic medication Topamax 50 mg twice daily with no clear monitoring of his seizures. The diagnosis of DWV was made by the neurologist as an outcome of the investigation and report of a Brain Magnetic Resonance Imaging (MRI) done at the age of 12 years showing: Absent left cerebellar hemisphere and severely dysplastic right cerebellar hemisphere, and vermis with large retro-cerebellar Cerebro- Spinal Fluid (CSF) cyst, supratentorial Ventriculomegaly (VM) with thinning of carpus callosum along with dysmorphic right hippocampus with suggestion of right temporal lobe atrophy (Figure 1).
The initial psychiatric assessment was done taking relevant history and collateral information from the patient, his parents and reviewing his electronic medical records. His parents described uncontrolled episodes of severe destructive behaviors, breaking Television screens, and his parents tend to buy two new televisions every month. He was reported to breaking cars, door handles and plates frequently. He forcefully takes his siblings’ belongings and breaking them while keeping his own items safe and not allowing other to reach them. Moreover, he was developing frequent and sudden episodes of aggression/assault towards strangers, neighbors and family members for no apparent reason. The parents reported that his siblings were injured during these episodes of aggression. With increasing social isolation, he refused to come out of his room and neglecting self-care along with few shouting episodes in anger if asked to self-care. He also showed sexually disinhibited behaviors towards female members of the family causing distress and avoidance His sleep has been disturbed as he wakes all night and only sleep for shot period during the day. There is no history of alcohol or drugs use and no family history of psychiatric illness.
His developmental history shows that he was born at 24 weeks gestation with a birth weight of 1.4 kg and G6DP deficiency. His postpartum periods were complicated by Neonatal Intensive Care Unit (NICU) admission and need for intubation along with incidence of intraventricular hemorrhage. He had febrile convulsions, chronic lung disease and Patent Ductus Arteriosus that was operate on at age 3 years. In addition, he had global developmental delay in cognitive and motor skills. He started speaking at 2 years of age and walked after the second year. He became dry by day at 4 years of age and needed significant support to achieve toilet training. Although attended mainstream school initially, however he has been supported all through with limited academic achievements. His education was interrupted by his behaviors and physical health issues needing to attend hospital appointments. He graduated from high school through special needs support educational program with poor academic performance.
In his mental state examination, when visited at the Emergency Department, he appeared slightly distressed, wearing night clothing, looking suspicious and was not cooperative to interview. He was nervous and shy asking to leave the room avoiding answering questions. He had fleeting eye contact and attempting to leave the room. His speech was clear, slow but with low tone and volume with delayed response. He appeared moody, irritable and his affect was changing, while being reactive only when talking about his interests. He holds paranoid ideas claiming that he is been watched and all people are against him wants to harm him but unable to expand but denied any hallucinations and suicidal or homicidal ideation. He appeared to have some insight into his behavior but not admitting to taking responsibility.
Neurological and general physical examination was unremarkable. Blood Investigations including; complete blood count testing, blood chemistry, thyroid function tests were within normal range and Electrocardiogram (ECG) was normal. He was referred for Neurologist review and a repeat electroencephalography which showed abnormal epileptiform discharges on the left posterior parietal region.
His behavior was managed using medical and nursing interventions and support from his family. His presentation was discussed with the neurologist and diagnostic formulation of organic psychosis in the contest of uncontrolled epilepsy was agreed. A plan to optimize his antiepileptic medication and use of small dose antipsychotic medication has been agreed. A behavioral approach to support the risk management plan and offer of short hospital admission was made. His family agreed with management plan except for the admission as he started to settle in the ED following the introduction of antipsychotic and expressed need to try treatment at home. Nursing and Occupational Therapy involvement to complete assessments of his need for support and monitoring of his medication at home agreed. His medication was adjusted with a to gradually withdraw Topiramate and introduce Sodium Valproate and use small dose Risperidone, psychoeducation given. He was visited at home for follow up by the Intellectual Disability team and he showed evidence of recovery whiting three weeks of discharge with significant reduction in his behavior and improved mental state.
Results and Discussion
The cerebellum is traditionally known to be primarily involved in regulation of coordination and motor functions. However, research indicates its potential role in sensory, procedural, linguistic actions along with its effect on irritability, affect, anger, aggressive behavior, and abnormal crying and/or laughter [21,22]. Previous clinical studies reported that stimulation of the surface of the vermis enhanced control of emotions and decreased aggressive bouts and feelings of anger [23,24]. Hence, cerebellar malformations; especially vermin hypoplasia are suggested to be significantly associated with anger, increased attacks of aggression, abnormal mood.
In this paper, we summaries radiological features, psychiatric manifestations and other mental health diagnoses in a group of 18 cases with DWS, with a special focus on the variant form of the disease (Table 1). Interestingly, only 6/18 cases reported aggressive/hostile behaviors with vermin hypoplasia or cerebellar hemisphere hypoplasia [15] being a common radiological feature. However, none of them seemed to have similar severity in the abusive, assaultive and destructive behaviors in our case; suggesting that absence of one cerebellar hemisphere and/or temporal lobe atrophy and/or thinning of the corpus callosum might further substantiate the severity of the behavioral presentation.
| Authors | Radiological features | Psychiatric symptoms | Diagnoses | Authors | Radiological features | Psychiatric symptoms | Diagnoses | |
|---|---|---|---|---|---|---|---|---|
| Marques et al. (2019) | Vermian hypoplasia | Irritability | DWV | Marques et al. (2019) | Vermian hypoplasia | Irritability | DWV | |
| Mega cisterna magna | Impulsive behavior | Schizophrenia | Mega cisterna magna | Impulsive behavior | Schizophrenia | |||
| Persecutory delusions | mental retardation | Persecutory delusions | mental retardation | |||||
| Dawra et al. | Vermian hypoplasia | Abusive behavior | DWV | Dawra et al. | Vermian hypoplasia | Abusive behavior | DWV | |
| (2017) | Fourth ventricle communication with cisterna magna | Decreased self-care | Mental retardation | (2017) | Fourth ventricle communication with cisterna magna | Decreased self-care | Mental retardation | |
| Inappropriate laughter/crying | Inappropriate laughter/crying | |||||||
| Sinha et al. (2017) | Vermian hypoplasia | Grandiose delusions | DWV | Sinha et al. (2017) | Vermian hypoplasia | Grandiose delusions | DWV | |
| Fourth ventricle communication with cisterna magna | Auditory hallucinations | Schizophrenia | Fourth ventricle communication with cisterna magna | Auditory hallucinations | Schizophrenia | |||
| Moderate impairment in memory | Borderline intelligence | Moderate impairment in memory | Borderline intelligence | |||||
| Rohanachandra et al. (2016) | Cerebellar hemispheres hypoplasia | Aggression | DWV | Rohanachandra et al. (2016) | Cerebellar hemispheres hypoplasia | Aggression | DWV | |
| Fourth VM | Sextual impulses | Schizophrenia w/ obsessive compulsive symptoms | Fourth VM | Sextual impulses | Schizophrenia w/ obsessive compulsive symptoms | |||
| CSF filled cleft connected to right sigmoid sinus | Delusions of grandiosity/control | CSF filled cleft connected to right sigmoid sinus | Delusions of grandiosity/control | |||||
| Somatic hallucinations | Somatic hallucinations | |||||||
| BATMAZ et al. (2016) | Third & fourth VM | High speed of thoughts | DWM | BATMAZ et al. (2016) | Third & fourth VM | High speed of thoughts | DWM | |
| Posterior fossa cyst | Grandiose attitude | Bipolar disorder | Posterior fossa cyst | Grandiose attitude | Bipolar disorder | |||
| Cerebellar hypoplasia | Borderline intelligence | Cerebellar hypoplasia | Borderline intelligence | |||||
| Zincir et al. (2014) | Vermian hypoplasia | Persecutory delusions | DWV | Zincir et al. (2014) | Vermian hypoplasia | Persecutory delusions | DWV | |
| Fourth VM | Auditory hallucinations | Schizophrenia | Fourth VM | Auditory hallucinations | Schizophrenia | |||
| Borderline intelligence | Borderline intelligence | |||||||
| Buonaguro et al. (2014) | Vermian hypoplasia | Persecutory delusions | DWV | Buonaguro et al. (2014) | Vermian hypoplasia | Persecutory delusions | DWV | |
| Enlarged cisterna magna | Cognitive deficits | Delusional Disorder | Enlarged cisterna magna | Cognitive deficits | Delusional Disorder | |||
| Fourth VM | Bipolar Disorder | Fourth VM | Bipolar Disorder | |||||
| Schizoaffective Disorder | Schizoaffective Disorder | |||||||
| Kim et al. (2013) | Vermian hypoplasia | Abusive/impulsive behavior | DWV | Kim et al. (2013) | Vermian hypoplasia | Abusive/impulsive behavior | DWV | |
| Enlarged cisterna magna | Major depressive disorder | Enlarged cisterna magna | Major depressive disorder | |||||
| General VM | General VM | |||||||
| Ryan et al. (2012) | Mild VM | Paranoid ideation | DWV | Ryan et al. (2012) | Mild VM | Paranoid ideation | DWV | |
| Pominence of basilar cisterns | Auditory hallucinations | Schizophrenia | Pominence of basilar cisterns | Auditory hallucinations | Schizophrenia | |||
| Prominent CSF space dorsal and inferior to the cerebellum | Prominent CSF space dorsal and inferior to the cerebellum | |||||||
| Ganet al. (2012) | Cerebellar vermis agenesis | Auditory hallucinations | DWM | Ganet al. (2012) | Cerebellar vermis agenesis | Auditory hallucinations | DWM | |
| Encephalatrophy | Persecutory delusions | Schizophrenia | Encephalatrophy | Persecutory delusions | Schizophrenia | |||
| Disinhibition | Disinhibition | |||||||
| Hypoplasia of cerebellar hemispheres and vermis | Restlessness | DWV | Hypoplasia of cerebellar hemispheres and vermis | Restlessness | DWV | |||
| Unreasonable phobia | Unreasonable phobia | |||||||
| Uncontrollable worries without reasons | Uncontrollable worries without reasons | |||||||
| Mega cisterna magna | Auditory hallucinations | Schizophrenia | Mega cisterna magna | Auditory hallucinations | Schizophrenia | |||
| Ischemic foci in frontal, temporal, and parietal lobes | Persecutory delusions | Mega cisterna magna | Ischemic foci in frontal, temporal, and parietal lobes | Persecutory delusions | Mega cisterna magna | |||
| Jealousy | Jealousy | |||||||
| Posterior fossa arachnoid cyst | Agitation and distraction | Posterior fossa arachnoid cyst | Posterior fossa arachnoid cyst | Agitation and distraction | Posterior fossa arachnoid cyst | |||
| Loss of interest | Mild mental retardation | Loss of interest | Mild mental retardation | |||||
| Repetitive behavior | Repetitive behavior | |||||||
| Delusions | Delusions | |||||||
| Aimua et al. (2012) | Vermian hypoplasia | Aggressive behavior | DWV | Aimua et al. (2012) | Vermian hypoplasia | Aggressive behavior | DWV | |
| Fourth VM | Bipolar disorder | Fourth VM | Bipolar disorder | |||||
| Communication between cisterna magna and fourth ventricle | Communication between cisterna magna and fourth ventricle | |||||||
| Lingeswaran et al. (2009) | Vermian hypoplasia | Excessive cheerfulness | DWV | Lingeswaran et al. (2009) | Vermian hypoplasia | Excessive cheerfulness | DWV | |
| Posterior fossa cyst | Disinhibited in speech/behavior, | Bipolar affective disorder | Posterior fossa cyst | Disinhibited in speech/behavior, | Bipolar affective disorder | |||
| Mega cisterna magna | Restlessness | Mega cisterna magna | Restlessness | |||||
| Disobedience | Disobedience | |||||||
| Prakash et al. (2009) | Vermian hypoplasia | Overactivity | DWV | Prakash et al. (2009) | Vermian hypoplasia | Overactivity | DWV | |
| Fourth VM | Abusive/destructive behavior | ADHD | Fourth VM | Abusive/destructive behavior | ADHD | |||
| Lying and stealing | Hyperkinetic conduct disorder | Lying and stealing | Hyperkinetic conduct disorder | |||||
| Mild mental retardation | Mild mental retardation | |||||||
| Papazisis et al. (2007) | Vermian hypoplasia | Severe delusional ideas | DWV | Papazisis et al. (2007) | Vermian hypoplasia | Severe delusional ideas | DWV | |
| Fourth VM | Auditory hallucinations | OCD | Fourth VM | Auditory hallucinations | OCD | |||
| Mild general VM | Schizophrenia | Mild general VM | Schizophrenia | |||||
| Mild mental retardation | Mild mental retardation | |||||||
| Turner et al. (2001) | Vermian hypoplasia | Hostile behavior | DWV | Turner et al. (2001) | Vermian hypoplasia | Hostile behaviour | DWV | |
| Cystic Fourth VM | Paranoid ideation | Schizophrenia | Cystic Fourth VM | Paranoid ideation | Schizophrenia | |||
Table 1: DWS: Case Reports with Radiological and Behavioural Features [5,6,8,9,10,12,14,16,17,13,18,20].
Schizophrenia was a common psychiatric comorbidity with DWS [7-11,15-20]. Marques et al. [17] reported that some patients can present with schizophrenia-like symptoms and might live up to 20 years with missed diagnosis of DWS that could have been reached via a simple brain imaging. Mental retardation was also fairly common with DWS, along with bipolar disorder [7,10,11- 14,16-19,8]. In our case we did not find features suggestive of psychosis, however the severity of his challenging behaviors might lead to use of antipsychotic medication as part of the risk management plan.
Conclusion
We highlight the need for multidisciplinary assessments and interventions from specialist services recognizing the support needed for families caring for such high intensity and severity challenging behaviors in adult cases. Such cases may need high level of support to engage in activities outside home environment and careers need to be trained on behavioral management approach to manage his risk and improve his quality of life.
Acknowledgments
This research did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
No conflicting relationship exists for any author.
Informed Consent
Written informed consent was obtained from the patient and his guardians for their anonymized information to be published in this article.
HMC Approval for Publication Obtained from the MRC
MRC-04-20-990
References
- Alsenani YS, Crosby GV, Ahmed KR, Velasco T (2020) ProTrust: A probabilistic trust framework for volunteer cloud computing. IEEE Access 8: 135059-135074.
- Barkovich AJ (1989) Revised classification of posterior fossa cysts and cystlike malformations based on the results of multiplanar MR imaging. AJR Am J Roentgenol 153(6): p. 1289-300
- McClelland S (2015) The natural history of Dandy-Walker syndrome in the United States: A population-based analysis. J Neurosci 6(1): p. 23-26
- Hirsch JF (1984) The Dandy-Walker malformation. A review of 40 cases. J Neurosurgeon 61(3): p. 515-22.
- Sasaki-Adams D (2008) The Dandy-Walker variant: A case series of 24 pediatric patients and evaluation of associated anomalies, incidence of hydrocephalus, and developmental outcomes. J Neurosurgeon Pediatr 2(3): p. 194-199.
- Kim JH (2013) Impulsive behaviour and recurrent major depression associated with dandy-walker variant. Psychiatry Investing 10(3): p. 303-305.
- Gan Z (2012) Psychosis and Dandy-Walker complex: Report of four cases. Gen Hosp Psychiatry 34(1): p. 102.e7-102.e11.
- Buonaguro EF, Cimmarosa S (2014) Bartolomeis AD Dandy-Walker syndrome with psychotic symptoms: A case report. Riv Psichiatr 49(2): p. 100-102
- Ryan M (2012) New-onset psychosis associated with dandy-walker variant in an adolescent female patient. J Neuropsychiatry Clin Neurosci 24(2): p. 241-6.
- Papazisis G, Mastrogianni A, Karastergiou A (2007) Early-onset schizophrenia and obsessive-compulsive disorder in a young man with Dandy-Walker variant. Schizophr Res 93(1-3): p. 403-405.
- Aimua F, Dunn NR, Swift GD (2012) Dandy walker variant with treatment-resistant bipolar disorder. J Neuropsychiatry Clin Neurosci 24(1): p. E50.
- Prakash R (2009) Psychiatry, Central Institute of Psychiatry, Udaipur, India, Psychiatric Comorbidities in Dandy-Walker Variant Disorder. J Neuropsychiatry and Clini Neurosci 21(4): p. 477-479.
- Dawra RD (2017) Psychosis in a Case of Dandy-Walker Syndrome: A Case Report. J Clin Diagn Res 11(5): Vd03-Vd04.
- Batmaz M (2017) Dandy-Walker Malformation Presenting with Affective Symptoms. Noro Psikiyatr Ars 54(3): 277-281.
- Rohanachandra YM, Dahanayake DM, Wijetunge S (2016) Dandy-Walker Malformation Presenting with Psychological Manifestations. Case Rep Psychiatry 2016: p. 9104306.
- Lingeswaran A, Barathi D, Sharma G (2009) Dandy-Walker variant associated with bipolar affective disorder. J Pediatr Neurosci 4(2): p. 131-132.
- Gama Marques J (2019) Twenty years of misdiagnosis of schizophrenia in a patient with Dandy-Walker variant syndrome. Gen Psychiatr 32(1): p. e100031.
- Sinha P (2017) Dandy-Walker Variant with Schizophrenia: Comorbidity or Cerebellar Cognitive Affective Syndrome? Indian J Psychol Med 39(2): p. 188-190.
- Bozkurt Zincir S (2014) Schizophrenia-like psychosis and dandy-walker variant comorbidity: Case report. Psychiatry Investig 11(1): p. 102-104.
- Turner SJ (2001) Schizophrenia-like psychosis and Dandy--Walker variant. Schizophr Res 48(2-3): p. 365-367.
- Schmahmann JD, Sherman JC (1998) The cerebellar cognitive affective syndrome. Brain 121( Pt 4): p. 561-79.
- Levisohn LA, Golomb C, Schmahmann JD (2000) Neuropsychological consequences of cerebellar tumour resection in children: cerebellar cognitive affective syndrome in a paediatric population. Brain 123 ( Pt 5): p. 1041-1050.
- Cooper IS (1976) chronic cerebellar stimulation in epilepsy. Clinical and anatomical studies. Arch Neurol, 1976. 33(8): p. 559-70.
- Heath RG (1977) Modulation of emotion with a brain pacemaker. Treatment for intractable psychiatric illness. J Nerv Ment Dis 165(5): p. 300-17.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences