Neuropsychiatric Problems such as Depression in Obese People and the Effects of COVID-19 Pandemic in these People
Lisha Singh*
Department of Medical Science, HMR Institute of Technology and Management, Haryana, India
- *Corresponding Author:
- Lisha Singh
Department of Medical Science, HMR Institute of Technology and Management, Haryana, India
E-mail: slisha127@gmail.com
Received: Sep 16, 2020, 2022, Manuscript No. IPJNP-20-6148; Editor assigned: Sep 22, 2020, PreQC No. IPJNP-20-6148; Reviewed: Oct 06, 2020, QC No. IPJNP-20-6148; Revised: June 28, 2022, QI No. Q- IPJNP-20-6148; Manuscript No. IPJNP-20-6148; Published: July 26, 2022
Citation: Singh L (2022) Neuropsychiatric Problems such as Depression in Obese People, and the Effects of COVID-19 Pandemic in these People. Neuropsychiatry Vol.6 No.3:001
Abstract
Introduction: Obesity is a very serious condition with brutal health impacts. This article summarizes recent clinical and psychological findings in this broad diseased area which will help researchers for better management. And the effects of COVID-19 pandemic on the obese patients and their associated mental health disorders (includes depression and anxiety).
Objective: The main view point of this review article is to lookout for the two clinical entities obesity and depression association.
Method: Selective reviews of the literature associated with obesity and includes areas like behavioural, and lifestyle by unfolding the deep relationship between psychotic illness and looking out for those obese patients suffering in this pandemic.
Conclusion: To spread awareness among individuals so that they can deal with this by changing various parameters of their life including quality, eating habits, physical health and most important mental health.
According to the epidemiological data of obesity, presents a major challenge to prevent this chronic disease across the globe. Obesity is a complex, multifactorial, and one of the medical conditions which is difficult to treat, affecting one third population of this world. If this trend continues, another 38% population would be overweight and 20% would be obese (according to the data provided).
Keywords
National obesity observatory; Hyperlipoidaemia; Leptin receptor; Melanocortin
Introduction
What is obesity and how commonly it is associated with psychotic illness?
Obesity is defined as Body Mass Index (BMI), calculated by dividing weight (in kilograms) by height (in meters) squared. Recent clinical guidelines developed by the National Heart, Lung, and Blood Institute define “overweight” as a body mass index of 25-29.9 kg/m2 and obesity as a body mass index of 30 kg/m2 and greater. Body mass index of 30-34.9 kg/m2 is classified as class I obesity, 35-39.9 kg/m2 as class II obesity, and 40 kg/m2 or more as class III or extreme obesity. Epidemiological studies show the direct relation between obesity and BMI [1].
Across the health agencies like WHO, have given data regarding the morbidity and mortality rates increasing with the people having BMI of 25 or more.
If we only talk about the obesity single handily, Obesity develops from a combination of environmental and genetic factors, both these factors can highly persist in obese people.
The reasons which link the obesity with psychiatric problems are very common: Poor self- image, physical inactivity, and social stigma associated with their shape of the body which increases the rate of mental illness more in obese people than normal or healthy individuals. This is not even right to call normal shape people to be healthy because various studies reveal that even the normal acting person is more likely to develop the cardiovascular problems (maybe some genetic factors).
Getting back to our concerned topic, Depression and low selfesteem have been observed in obese patients around the world, even when there is no previous history of mental illness. Studies conducted at the Texas Health Science Center and by the UK’s National Obesity Observatory (NOO) are among the many research programs confirming that the obese are at greater risk for depression [2].
Literature Review
Impact of obesity on individuals and society
Obesity is a chronic disorder and serious health issue. The literature which have presented the proofs of links between obesity and increasing other health problems are like hypertension, hyperlipoidaemia, coronary artery disorder, gallstone, lipomas, and to be specific with women are infertility, irregular menstrual cycles, and increased pregnancy risks.
The BMI rate for overweight tells about the modestly mortality, class 1 obesity BMI rate for the markedly increase in mortality and severe obesity concludes for other higher BMI rates. Even the literature shows that the fat accumulated near the abdominal region of body account for the direct relation with the BMI rate increase [3].
The distilled effects are not only seen medically, but also socially as well. The society in which we live, enforce their judgmental comments on the obese people in every aspect of their life which includes marriage, job seeking, even on their appearance etc.
Causes and maintenance of obesity
Obesity is the most complex and multifactorial order which mainly accounts for genetic and environmental factors.
Genetic behind Obesity
The experimentation done on single gene animal models of obesity revealed the molecules responsible are leptin, the leptin receptor, agouti signalling protein and carboxypeptidase E, POMC (pro-opiomelanocortin) deficiency, MC4R (melanocortin 4 receptor) deficiency. And also studies show that these can be fully supporting the maintenance of obesity in Humans [4].
People who have obesity or started to grow above their normal weight in childhood, they have multiple genes which predispose them to gain weight. For example, fat mass and Obesity associated gene (FTO). This gene is present in almost up to 43% population. If any individual does have this gene then it is likely to cause
• Increase hunger levels
• Increase caloric values
• Decreased satiet
• Reduced control over eating
• Increased tendency to store food and fat
It is not likely to happen if you have these genes then you are predestined to have obesity, instead it is completely depending on your lifestyle as well.
Environment behind obesity
Several scientists believe that obesity is more influenced by environmental factors like high food consumption, high sweetened beverages, less activity outdoors, television watching etc., instead of biological ones.
Even, nowadays due to social globalization, we are everyday influenced by the interesting posters and pictures of food items which offers high calorific value and fat content. Furthermore, our environment has been sliding to more towards obesogenic environment and encouraging us to eat more unhealthy stuffs [5].
Today’s time is completely opposite from the past, where human used to engage themselves in outdoor activities which were regulating the expenditure and intake of energy in a more proper way.
What is depression and how it is caused?
It is a mental health disorder characterized by persistently depressed mood or loss of interest in activities, causing significant impairment in daily life.
Possible causes include a combination of biological, psychological and social sources of distress. Increasingly, research suggests that these factors may cause changes in brain function, including altered activity of certain neural circuits in the brain. The persistent feeling of sadness or loss of interest that characterizes major depression can lead to a range of behavioral and physical symptoms. These may include changes in sleep, appetite, energy level, concentration, daily behavior or selfesteem. Depression can also be associated with thoughts of suicide [6].
The mainstay of treatment is usually medication, talk therapy or a combination of the two. Increasingly, research suggests that these treatments may normalize brain changes associated with depression.
Depression is diagnosed in to almost 4% of the world population, with 16.6% lifetime prevalence which has great social and public health.
The neurobiological models of depression show the dependency on individual predisposition and activation of serotonergic pathway and reduces the serotonin availability.
The literature on the association between obesity and depression provide the relevance of hypothalamic pituitary adrenal axis dysfunction, Sympathetic Nervous system (SNs) activation, glucocorticoid production, inflammatory processes with the interaction of genetic and environmental factors [7].
How people are more likely to develop depression with obesity or vice-versa?
Studies have found depression to correlate with the onset of obesity and obesity to predict the onset of depression depression predicts poor success with weight loss, but successful weight is greatly linked to reduction in depression.
Male or female
In a comparative study of psychologist, it says that women’s, who are less emotional positive are at a greater risk of weight gain than the men in the same context.
When we talk about the differences between two opposite genders many parameters fall into this like, the emotional status, work load, biological problems, etc [8].
Obesity is vice versa related to depression, either it is in male or female
Males are prone to depression when they are overweight and likely to develop some serious health conditions as well like prostate cancer and so on. As of the studies we know, Men are at lower risk of developing depression or anxiety because the fat which is responsible for the imbalance of HPA axis lies in the abdominal area. Women’s are 5% more prone to these psychological conditions because of their increased and residence fat in abdominal area.There is even some evidence that overweight and obesity may be associated with a lower likelihood of attempting or committing suicide among men, although increased BMI is associated with a greater likelihood of suicidal ideation among women.
Mood and anxiety disorders lead to weight gain by interfering into the healthy eating habits and regular exercise.
Women are more likely to eat when she faces any kind of negative emotion than men, which shows an increased appetite as one of the symptoms of depression.
Substance use disorders or psychotropic medications?
Weight gain is one of the problematic side effects of psychotropic medications used by mentally ill patients. And medications include antipsychotics, antidepressants, mood stabilizers and anxiolytics. And when weight gain becomes chronic because these medications need to be taken frequently, the patients become obese.
And the direct relation of obesity is under the mechanism responsible for inhibition of histamine H2, serotonin 5-HT, and Dopamine D2 receptors.
However, as reviewed, more recent studies have reported relatively modest mean weight gains, even over the long term, and much larger increases in a relatively small number of patients. Of the tricyclics, amitriptyline is thought to induce the most weight gain. The mechanism of tricyclic antidepressantinduced weight gain appears to involve decreased basal metabolic energy expenditure and diet-induced thermogenesis. Shifts in food preference toward calorically dense foods occur in a minority of patients but do not seem to be associated with significant weight gain.
According to Epidemiological studies, the relation between obesity and substance use disorders came out with inconsistent reports. The findings says, the there is an association between lifetime alcohol use disorder with the BMI of individuals. And men are more likely to develop obesity than the women.
The mechanism is as follows: Intake of food or drugs is reinforcing which activates reward circuiting in the brain and releases Dopamine. A reward response towards more greasy food encourages eating thus for survival, but which also leads to obesity in chronic substance use of drugs. Overeating might be a one of the response behaviours shown because of activation of hypoactive dopamine system [9].
Treatment of psychosocial behavior of obese patients
Obese patients and their health care providers may readily conclude that any distress patients experience is attributable to their size and that they “just need to lose weight.” Clinicians are cautioned, however, against assuming that obese people who suffer from significant depression are depressed because theyare obese. The vast majority of obese people, in fact, are not depressed. Those who do have a mood disorder deserve and require the same care that would be provided to a depressed person of average weight.
We recommend that patients with major depression be treated for their mood disturbance before weight loss is undertaken. The cognitive and behavioural symptoms of depression (e.g., poor concentration, low motivation, social withdrawal) can diminish patients’ capacity to adhere to a weight loss program, leaving them vulnerable to attrition, unsatisfactory weight loss, and exacerbation of the mood disorder.
Obesity and depression-neuro-inflammatory and endocrine pathways involved
Recent research shows that there is an involvement of regulatory systems in obesity i.e. White Adipose Tissue (WAT).
When the experiments were conducted in animal models, stress in the body releases Neuropeptide Y, which promotes the differentiation of adipocytes and angiogenesis in the presence of high fat and sugar diet. When there is a prolonged activation of this Neuropeptide Y results in increase of adipose tissue and metabolic syndrome. And adipose tissue being considered as an endocrine organ communicating between peripheral organs and central nervous system.
Continuous inflammation leads to increase in adipose tissue size, due to pro-inflammatory cytokines such as TNF-α and IL-6, which is produced by adipose tissue, which explains the neuroendocrine activation and glucose metabolism changes observed in obesity. Now all these activation changes in body, results in HPA axis hyperactivation provoke obesity in two pathways: Homeostatic pathway includes suppression of Corticotrophin Releasing Hormone (CRH), resistance to leptin, and increase in NPY release. And the second non-homeostatic pathway includes food associated reward and pleasure promotes a shift to high calorific diet. Depression and Obesity both have common neurobiological pathway, which tells about the stress induced responsible for both the comorbidities. Stress induces the release of proinflammatory cytokines in response to inflammation and hyperactivation of HP Axis. The simple relation lies between two i.e. Stress caused in white adipose tissue causes obesity and stress in CNS causes depression.
An important role of leptin, adiponectin and resistin have been shown in recent research have a connection with the neuropsychiatric disorders associated with metabolic abnormalities. Nevertheless, the link between obesity and depression is still under research.
Effects of COVID-19 pandemic in these obese people
Coronavirus disease-2019 (COVID-19) is an infectious disease caused by newly discovered coronavirus. Coronaviruses are group of related RNA viruses that causes diseases in mammals and birds (as far discovered). In humans these viruses causes respiratory tract infections which can range from mild to lethal even death, Mild symptoms can be like common cold (as it isspread by most of the common viruses), and severe illness like SARS, MERS, and COVID-19.
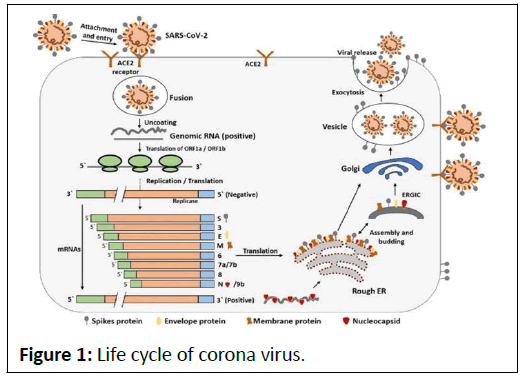
As far the biology of Coronavirus is concerned, Coronavirus belongs to the family of Orthocorovirinae. They are enveloped viruses with a positive sense single stranded RNA genome and nucleocapsid helical symmetry. It is wrapped in icosahedral protein shell. The size of the virus ranged from 26-32 kilobases and have characteristic club shaped spikes on their surface as discovered by the electron micrograph images (Figure 1).
Transmission of coronavirus
Coronavirus can be transmitted by droplets of different sizes, which are called as respiratory droplets of size 5 μm-10 μm. According to the current evidence and WHO findings, COVID-19 virus is primarily transmitted between people through respiratory droplets and contact routes.
The COVID-19 virus spreads primarily through droplets of saliva or discharge from the nose when an infected person coughs or sneezes [10].
The effects of COVID-19 on obese people
If we talk about the normal health of Obese people, which is at risk because, the more overweight you are, the more fat you are carrying , the less fit you are and which lowers the capacity of lungs which means the body struggle too much to get sufficient oxygen. This happens, because the body is undergoing so much of pressure and finding it very difficult to complete the hunger of blood oxygen.
When an infectious disease like coronavirus, obese people are at higher risk of getting this disease, eventually the obese body becomes overwhelmed by the lack of oxygen getting to the major organs. This is the only reason why obese people are more likely to get assistance with the breathing and intensive care support system. Scientists have discovered an enzyme called ACE2, which is the prominent pathway for the virus to enter inside the host organism. The obese people have higher levels of this molecule inside their adipose tissue or fatty tissue, especially near the internal organs.
Discussion
As much as the obese people are concerned, their BMI also give so much of relevance. There is a study from John Hopkins Hospital, those patients who are admitted because of pandemic, needs higher rate of instrumental help who are obese. And the shocking fact is this, the young people are more prone to this disease because of their BMI don’t lie in their proximity. The effects of COVID-19 have a drastic influence on normal/healthy individual, because of lockdown situation, social distancing, not able move out from their houses, binge eating all the time, and there is no expenditure of energy they are getting from the home cooked food. Our concern is the mental health of obese patients is that, those who are already under medications for depression, they are facing a lot of stressful; suffocating situation inside their own body. Because as the study says, depressed patients have to be more in contact with nature so that the neuropsychological molecules can come under the control.
Conclusion
The obesity, with depression making it very hard for the individuals to work from home, engage in physical activity because of their heavy weight, tiredness. Even these conditions making it worse for them when something happen with them emotionally. They are not in a condition to go through all this because of their complexity and imbalances of hormones. The obese patients are facing a lot of bodily changes like in females, there is a drastic change in the menstrual cycle, emotional stress, tiredness, low productivity, and negativity. While in males, there is a lot more stress has the role to play which leads to anger issues, low productivity, not manageable emotional stress, even the studies say, in general the stress leads to decrease in the motility rate of sperms. The above review article is to make awareness among the individuals regarding their health, so that preventive measures for coronavirus and for their mental health issue can be taken. Because the long-term effects of this pandemic would be very serious on those who are already under medications.
References
- David Engstrom (2007) Obesity and depression. Spring 3.
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, et al. (2010) Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 67: 220-229.
- Simon GE, Ludman EJ, Linde JA, Operskalski BH, Ichikawa L, et al. (2008) Association between obesity and depression in middle-aged women. Gen Hosp Psychiatry 30: 32-39.
- Linde JA, Simon GE, Ludman EJ, Ichikawa LE, Operskalski BH, et al. (2011) A randomized controlled trial of behavioral weight loss treatment versus combined weight loss/depression treatment among women with comorbid obesity and depression. Ann Behav Med 41: 119-130.
- Devlin MJ, Yanovski SZ, Wilson GT (2000) Obesity: what mental health professionals need to know. Am J Psychiatry 157: 854-866.
- Ouakinin SR, Barreira DP, Gois CJ (2018) Depression and obesity: Integrating the role of stress, neuroendocrine dysfunction and inflammatory pathways. Front Endocrinol 9: 431.
- Nakamura ZM, Nash RP, Laughon SL, Rosenstein DL (2021) Neuropsychiatric complications of COVID-19. Curr Psychiatry Rep 23: 1-9.
- De Sousa RAL, Improta-Caria AC, Aras-Júnior R, de Oliveira EM, Soci ÚPR, et al. (2021) Physical exercise effects on the brain during COVID-19 pandemic: Links between mental and cardiovascular health. Neurol Sci 42: 1325-1334.
- Hao F, Tam W, Hu X, Tan W, Jiang L, et al. (2020) A quantitative and qualitative study on the neuropsychiatric sequelae of acutely ill COVID-19 inpatients in isolation facilities. Transl Psychiatry 10: 1-14.
- Villapol S (2020) Gastrointestinal symptoms associated with COVID-19: Impact on the gut microbiome. Transl Res 226: 57-69.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences