The Link between Alzheimer Disease and Sleep Quality
Oussama Gaied Chortane1*, Imen Ben Amar2, Sofien Amara2, Hajer Aouani2 and Patricia Cristine Heyn2
1Department of Human and Social Sciences, University of Manouba, Tunis, Tunisia
2Department of Health and Society, University of Manouba, Tunis, Tunisia
- *Corresponding Author:
- Oussama Gaied Chortane
Department of Human and Social Sciences,
University of Manouba,
Tunis,
Tunisia,
Tel: 21625909620;
E-mail: oussama.gaeid@gmail.com
Received date: November 12, 2022, Manuscript No. IPJNP-22-14859; Editor assigned date: November 15, 2022, PreQC No. IPJNP-22-14859 (PQ); Reviewed date: November 30, 2022, QC No. IPJNP-22-14859; Revised date: January 20, 2023, Manuscript No. IPJNP-22-14859 (R); Published date January 27, 2023, DOI: 10.36648/2471-8548.23.07.001
Citation: Chortane OG, Amar IB, Amara S, Aouani H, Heyn PC (2023) The Link between Alzheimer Disease and Sleep Quality. J Neuropsychiatry Vol: 7 No:1
Abstract
Sleep problems are common in institutionalized elders and are associated with increased mortality and morbidity. Recent research has proved that sleep disturbances and circadian rhythm have been related to the pathophysiology of Alzheimer's disease and would influence the progression of the pathology and lead to both cognitive and noncognitive disabilities. We look at the current research that supports the idea that the lack of sleep relates to cognitive disorders and dementia, with an emphasis on Alzheimer's disease. We integrated multitude possible mechanisms of sleep deprivation leading to Alzheimer’s disease and cognitive decline. The role of neuroinflammation, circadian rhythm and sleep disturbances play a basic role in tau generation and Aβ deposition. An approach to manage sleep changes can widely prevent and delay the cognitive decline of Alzheimer’s disease. This review brings together the various possible mechanisms of how sleep disorders can lead to cognitive dysfunction and how the nonpharmacological treatment can delay the progression of sleep dysfunction in older patients.
Keywords
Alzheimer’s disease; Sleep problems; Cognitive functions; Aged patients; Neuroinflammation
Introduction
Alzheimer’s Disease (AD) is an age related and irreversible neurodegenerative brain disease [1]. It is generally known that the majority of Alzheimer’s patients have sleep problems, which affect the quality of life and well being [2]. Older people have increased prevalence of sleep disorders secondary to physiological decline in their circadian sleep rhythm [3]. This reflects the importance of sleep control for those elderly patients whose living in chronic care hospitalization and characterized by frailty, cognitive impairment decreased physical activity and increased prevalence of specific sleep disorders compared to normal population [4]. Initially, there is a great evidence relationship between sleep problems and neurodegenerative disease, recent studies suggest that sleep problems can show up years before cognitive disorders and thus become a plausible biomarker for early prevention and diagnostic intervention [5]. The term "sleep quality" refers to how well you sleep. Sleep quality is defined as a person's contentment with their sleep experience, which includes factors such as sleep initiation, sleep maintenance, sleep quantity, and wakefulness. Sleep quality is more difficult to measure and to quantify than sleep quantity, although it is not completely subjective. Generally, sleep quality is usually measured using four criteria:
Sleep latency: The length of time it takes the person to fall asleep is known as sleep latency. Sleeping off within 30 minutes or less of going to bed is found to be one of the indicators that sleep is of good quality.
Sleep waking: The frequency with which the person wakes up during the night is measured by sleep waking. Frequent waking is seen as an indicator of poor sleep.
Wakefulness: The number of minutes person is awake during the night after people first go to sleep is referred to as wakefulness. The higher the time of wakefulness the poorer the sleep quality.
Sleep efficiency: Sleep efficiency refers to the amount of time people spend sleeping when in bed. The higher the time the time the better the sleep quality [6].
Literature Review
Theories of sleep
Restorative theory: According to the restorative idea, sleep permits the body to revitalize and restore the physiological process required to rejuvenate the body and mind [7]. Numerous biological functions, such as muscle repair, clearing waste toxins from the brain regions, protein synthesis, repairing tissues throughout the body, and the release of many important growth hormones, are shown to occur largely during and the release of many important growth hormones, are shown to occur largely during sleep [8].
Adaptive theory: Also called the evolution theory or preservation theory is also known as the inactivity theory of sleep. A flaw in this theory, scientific studies showed that sleeping limits productivity, such as finding food and reproducing, so staying awake longer would be an evolutionary benefit [9]. Sleepiness, like hunger and thirst, may indicate an underlying physiological need that can only be met by sleeping and is critical to an individual's survival.
Sleep and mental health: Sleep and mental health are closely connected. Sleep disorders affects psychological state and mental well being. Sleep deprivation has been found to be one of the important causes of a range of negative health outcomes, including, Alzheimer disease, heart disease, type 2 diabetes, and depression. At the same time, sleep disorders can be caused by psychiatric ailments, and abnormalities in sleep can increase the symptoms of many mental illnesses, including depression, anxiety, and bipolar disorder. Sleep has long been recognized as a symptom of many psychiatric and neuropsychological disorders, newer theories imply that sleep can also play a causative role in the development and maintenance of mental illnesses [10].
Sleep deprivation and Amyloid Beta (Aβ) protein: Assuming that AD pathophysiology occurs quietly many years before the manifestation of cognitive disorders, recent scientific data show that research in neuroscience is focusing on the preclinical stage of AD. The pathophysiology process of AD is based on the presence and the accumulation of extracellular Beta-Amyloid (Aβ) deposits. Beta-amyloid molecules play an important role in AD, which is triggered by both genetic and environmental factors, and there is an increasing accumulation of Aβ in all brain regions in patients with Alzheimer disease. Increasing Aβ mass causes neuronal cell death, loss of synapses, and leads to a progressive decreasing of brain volume, which affects most of cognitive and functional parameters [11]. Scientific studies in both academic and pharmaceutical industry have strongly verified the link between the amyloid cascade protein and the presence of Alzheimer disease [12].
It has recently been generally confirmed that the progression of the cognitive functions is relatively due to a high levels of inflammatory response in the brain in AD and high immune gene activation increases the susceptibility to neurodegeneration [13]. Many researchers studies have verified the relationship between sleep measurements, Aβ protein levels, and cognitive dysfunction in older patients, however, those studies has indicated that poor quality of sleep is related to a poor cognitive parameters. The abnormal accumulation of Aβ and tau proteins is a significant source of synaptic dysfunction, neurotransmission deterioration, and sleep problems, both of them playing a critical part in the development of Alzheimer's disease [14]. Changes in sleep seem to precede the onset of cognitive symptoms in patients with AD, and sleep quality decline further in parallel with both cognitive disorders and the progression of the chronic disease.
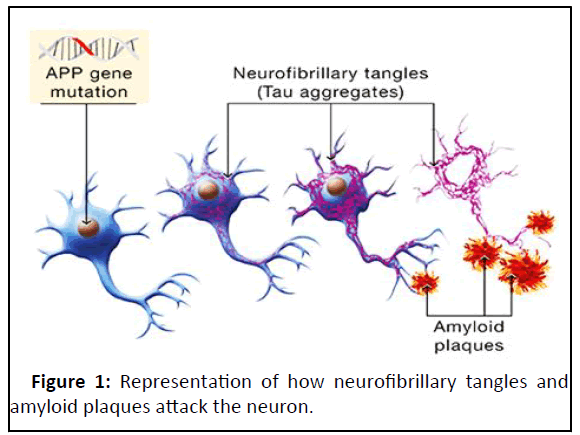
Tau protein homeostasis: Tau is one of the most important Microtubule Associated Proteins (MAP) in the neurons. The balanced tau phosphorylation binds it to the microtubules, assembles the microtubules, and maintains the structure and stability of the neurons [15]. However, the hyper phosphorylation state of tau facilitates the formation of intracellular tangles, which directly disrupts neuronal homeostasis and contributes to the cell death (Figure 1) [16]. Evidence from animal models illustrates that changes in the sleep wake cycle may increase hyper phosphorylated Tau protein in the brain [17]. Scientific studies have showed that two months of abnormal sleep, causes more than 50% elevation of the insoluble Tau in the brain and lead to increase the dysfunctional process of tau metabolism [18].
Epigenetic factors in Alzheimer’s disease
Epigenetics is the study of how cells control gene activity without changing the DNA sequence. The progression of AD occur with the interaction of various and different factors, such aging, genetic mutations, metabolic activity, and nutritional problems, as well as environmental and social interactions [19]. Recent advances in sequencing technologies have allowed for a large pool of studies investigating DNA methylation in Alzheimer pathology, However, DNA methylation is crucial in maintaining basic cellular mechanism and synaptic plasticity in central nervous system, affecting cognitive parameters. Decreased DNA methylation in brain regions can affect neural plasticity, prevents memory formation, and leads to memory loss with aging in AD patients.
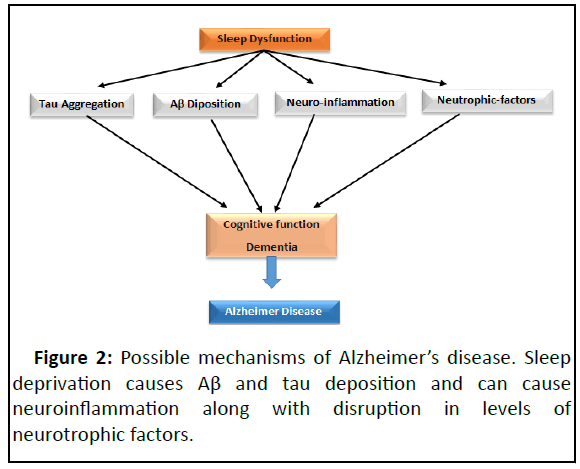
In addition to aging factor, cardiovascular diseases, which are other epigenetic risk factors, are the most frequently reported precursor factors of AD. In addition to all of these, the progression of AD is further enhanced by various variables including smoking, diabetes, hypertension, obesity, dyslipidemia (increasing blood cholesterol level), accidents brain injury, marital status, and psychologic functions (Figure 2).
Circadian rhythm and Alzheimer disease
Circadian alterations occur both during healthy aging and in age related diseases such as Alzheimer disease. There is a progressive deterioration of circadian rhythms with aging [20]. These include various modifications in the sleep wake cycle influenced by an important decreasing in sleep quality and cognitive impairment, and involve nocturnal sleep fragmentation, increased wakefulness, and decreased levels of daytime activity. These sleep disturbances have a significant impact on patients and their caregivers, and present a major risk factor for early institutionalization. There is good reason to detect problems in circadian rhythms in patients with dementia, especially those with Alzheimer’s disease.
The principal reason for the fluctuation in sleep wake cycle can be explained with the alterations in the Super Chiasmatic Nucleus (SCN) and melatonin secretion. At the cellular level, there is a decrease in the activity of neurons within the SCN in Alzheimer’s patients. It would be surprising not to find alterations in circadian rhythms for these patients, but one might expect problems to develop only at advanced stages of neurodegeneration. Nevertheless, contradictions results concerning the nature of circadian rhythms have been reported. Research’s about Alzheimer patients have showed worse, similar, and butter circadian temperature rhythms when compared with non-demented older patients.
Body clock disruptions
People with Alzheimer’s disease are known to have disturbances in their internal body clocks that affect the sleep/ wake cycle and may increase risk of developing the disorder. The biological clock is regulated and synchronized by the Supra Chiasmatic Nucleus (SCN) of the hypothalamus. It resets on a daily basis via light inputs from the retina during the day and melatonin secretion during the night. The SCN regulates and controlling the timing of humoral controls including sleep wake, temperature, and cognitive function by sending signals to numerous hypothalamic nuclei. The SCN regulates output pathways that affect different physiological parameters using two types neuronal and humoral signals. The proper timing of hormone release, feeding behavior, and body temperature changes is determined by these output pathways.
Potential therapeutic and treatments strategies
The aim of the treatment is to improve the quality of life of patients and caregivers. Because these conditions can have a major impact on quality of life, it seems logical to think that the treatment would also improve some cognitive domains. Authors have suggested a possible preventive effect for controlling the progression of Alzheimer disease. More research is needed to generate evidence based guidelines backed up by strong scientific evidence, but currently, the available therapeutic information’s offers some potential strategies discussed in the following paragraphs.
Nonpharmacological treatment
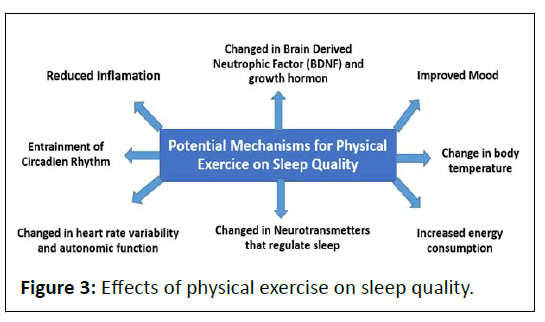
Physical activity: Exercise has shown potential for improving sleep dysfunction in AD as well. Given the possibility that exercise can be used to potentiate other circadian resynchronization methods, confirmed with potential evidence that leisure time physical activity is protective against AD. Most published research studies describes observational studies evaluating the relationship between physical activity and sleep in AD.
In cross sectional study, 59 patients with dementia evaluated with the mini sleep questionnaire, participants who following a regular physical training haw fewer sleep disorders compared to those who had lower levels of physical training. In another observational study, 183 patients with dementia examined the effects of physical activity based on walking hours per week on sleep quality. Results showed a significant improvement in sleep quality in patients with Alzheimer disease who practiced more walking hours. In summary, several studies suggest that exercise has the potential to improve sleep in persons with AD (Figure 3). Physical activity recommendations should be settled for controlling the progression of the disease for patients in all different stages of this chronic pathology and to determine the potential mechanisms underlying exercise induced changes in sleep.
Discussion
Sleep hygiene and environmental measures
The term ‘sleep hygiene’ refers to a set of behavioral and environmental recommendations intended to improve sleep quality. The basic advices of sleep hygiene include maintaining a regular sleep schedule, engaging in adapted daily exercises, minimizing daytime naps, minimizing and decreasing the use of caffeine, tobacco and alcohol, keeping the sleep environment dark, quiet, try to stay out from noise, and generally restricting light close to bedtime. Environmental factors contributes in change of sleep disorders that occur with age, that affect daily activities specially after retirement, mealtimes become irregular, pain and other comorbidities lead to increases the level of physical inactivity, while loneliness become more prevalent and that can also contribute to increase psychologic problems in patients with Alzheimer disease such as depression and anxiety.
Meal timing
It has been shown that eating timing, can prevent circadian disruption and even induce circadian resynchronization, however, research studies indicates that food timing can be a powerful synchronizing, or desynchronizing factor and affect circadian system through complex interplay of central and peripheral oscillators.
Bright light therapy
Bright Light Therapy (BLT) is a therapy used to treat sleep disorders. Research study have confirmed that 2 h of bright light therapy during 4 weeks improve the circadian rhythm in patients with Alzheimer dementia, most specifically it help to decreased day time sleep and increase night time sleep. These measures showed a reduction in day time sleepiness, a decrease in average duration and frequency of nocturnal awakenings, although one study found no significant change. The impacts of bright light therapy have been well studied; however, this technique applied at an intensity of greater than 2500 lux for half an hour or more in the morning or all day shows a various improvements in sleep quality.
Musical therapy
Music interventions have also been shown to have other positive physiological effects on AD persons that may affect cognition and behavior, such as improving sleep by increasing melatonin levels.
The musical therapy have gained an important increasing amount of interest in scientific studies, it’s a very accepted method and therapeutic technique, inexpensive, easily implemented, and highly enjoyable means of treatment for persons with Alzheimer disease. Behavioral studies concerning musical therapy intervention in AD indicate a good motivation level and high engagement in those with the disease and for the caregivers.
Conclusion
Sleep disturbances occur frequently in persons with Alzheimer disease, oftentimes increasing as the progression of severity of this disease increases. Changes in the brain region, in addition to normal changes in sleep because of aging as principal factor, add to the sleep disorders that are experienced by older patients with dementia. Evidence supports a strong relationship between sleep problems and Aβ and tau burden, meaning that sleep disruption might be both a cause and a consequence of neurodegenerative disease such as Alzheimer. Practice of sleep hygiene which encourages habits conducive to restorative sleep and avoidance of substances or behaviors that can affect sleep can help in resolving the problems associated with sleep disturbances to a very great extent. Understanding the sleep cycle of the individual, factors that significantly affect sleep and using a customized intervention model of psychological therapies can also help improving the sleep nevertheless, much needs still to be learned about these links, and subsequently improve treatment outcomes, decrease health distress experienced by both patients and caregivers providers and increase overall level of function. In individuals, there by alleviating the distress experienced because of it. This can also help in preventing the secondary effect on mental health issues such as anxiety and depression.
References
- Zhou Y, Song W, Andhey P, Swain A, Levy T, et al. (2020) Human and mouse single nucleus transcriptomics reveal TREM2 dependent and TREM2-independent cellular responses in Alzheimer's disease. Nat Med 26:131–142
[Crossref] [Google Scholar] [PubMed]
- Prinz PN, Vitaliano PP, Vitiello MV (1982) Sleep, EEG and mental function changes in senile dementia of the Alzheimer’s type. Neurobiol Aging 3:361-370
[Crossref] [Google Scholar] [PubMed]
- Vitiello MV, Moe KE, Prinz PN (2002) Sleep complaints cosegregate with illness in older adults: Clinical research informed by and informing epidemiological studies of sleep. J Psychosom Res 53:555-559
[Crossref] [Google Scholar] [PubMed]
- Gordon AL, Gladman JR (2014) Sleep in care homes. Review in Clinical Gerentology 20:309-316
- Rongve A, Boeve BF, Aarsland D (2010) Frequency and correlates of caregiver reported sleep disturbances in a sample of persons with early dementia. J Am Geriatr Soc 58:480-486
[Crossref] [Google Scholar] [PubMed]
- Xie L, Kang H, Xu Q (2013) Sleep drives metabolite clearance from the adult brain. Science 342:373–377
[Crossref] [Google Scholar] [PubMed]
- Ezenwanne E (2015) Current concepts in the neurophysiologic basis of sleep; a review. Ann Med Health Sci Res 1:173-179
[Google Scholar] [PubMed]
- Freiberg AS (2020) Why we sleep: A hypo thesis for an ultimate or evolutionary origin for sleep and other physiological rhythms. J Circadian Rhythms 18:2
[Crossref] [Google Scholar] [PubMed]
- Kinney JW, Bemiller SM, Murtishaw AS, Leisgang AM, Salazar AM, et al. (2018) Inflammation as a central mechanism in Alzheimer's disease. Alzheimers Dement 4:575-590
[Crossref] [Google Scholar] [PubMed]
- Karran E, Mercken M, de Strooper B (2011) The amyloid cascade hypothesis for Alzheimer’s Disease: An appraisal for the development of therapeutics. Nat Rev Drug Discov 10:698–712
[Crossref] [Google Scholar] [PubMed]
- Erbakan K, Doganoglu A, Erbas O (2021) Effects of lycopene on neurodegenerative diseases. JEB Med Sci 2:50-61
- Mander BA, Winer JR, Walker MP (2017) Sleep and human aging. Neuron 94:19-36
[Crossref] [Google Scholar] [PubMed]
- Kadavath H, Hofele RV, Biernat J, Kumar S, Tepper K, et al. (2015) Tau stabilizes microtubules by binding at the interface between tubulin heterodimers. Proc Natl Acad Sci USA 112:7501–7506
[Crossref] [Google Scholar] [PubMed]
- Iqbal K, Liu F, Gong CX (2016) Tau and neurodegenerative disease: The story so far. Nature Reviews. Nat Rev Neurol 12:15–27
[Crossref] [Google Scholar] [PubMed]
- Di Meco A, Joshi YB, Pratico D (2014) Sleep deprivation impairs memory, tau metabolism, and synaptic integrity of a mouse model of Alzheimer’s disease with plaques and tangles. Neurobiol Aging 35:1813–18120
[Crossref] [Google Scholar] [PubMed]
- Nunomura A, Perry G, Aliev G, Hirai K, Takeda A, et al. (2001) Oxidative damage is the earliest event in Alzheimer disease. J Neuropathol Exp Neurol 60:759–767
[Crossref] [Google Scholar] [PubMed]
- Sweatt JD (2013) The emerging field of neuroepigenetics. Neuron 80:624-632
[Crossref] [Google Scholar] [PubMed]
- Cui D, Xu X (2018) DNA methyltransferases, DNA methylation, and age associated cognitive function. Int J Mol Sci 19:1315
[Crossref] [Google Scholar] [PubMed]
- Giri M, Zhang M, Lu Y (2016) Genes associated with Alzheimer's disease: An overview and current status. Clin Interv Aging 11:665-681
[Crossref] [Google Scholar] [PubMed]
- Meraz-Rios MA, Guevara-Guzman R, Carvajal KG, Campos-Pena V (2016) Editorial: Neurodegeneration: From Genetics to Molecules. Front Cell Neurosci 10:187
[Crossref] [Google Scholar] [PubMed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences